Cystic fibrosis (CF) is a genetic disease that causes lung infections and other abnormalities which lead to premature death. Thousands of different genetic mutations have been identified as being responsible for CF, and recently scientists have developed new drugs that are effective for patients with some of the mutations. By identifying specific genetic defects in CF patients and developing therapies that can be deployed to those individuals who can best respond, medical research has given new hope to CF patients. This is one of an increasing number of examples of precision/personalized medicine (PM).
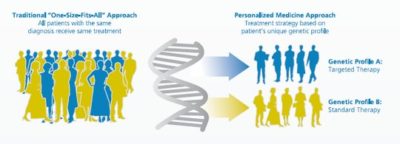
Courtesy of the Personalized Medicine Coalition
Precision medicine focuses on the goal of developing tailor-made treatments based on the genetic makeup and other individual characteristics of the particular patient being treated. Instead of the "one size fits all" paradigm, physicians choose treatments that are customized to the patient after consideration of their genetic, environmental and behavorial characteristics. Its aim is to move away from treatments designed to work for the "average patient", which are successful for some but not all, and to develop treatments and prevention strategies that take into account differences in people's genes, environments and lifestyles.
This approach has been further extended by some to systems medicine (SM) in which interventions are designed even before disease manifests. In SM, the strategy is to accumulate all the molecular, clinical and other personal data about the individual, and use this to provide advice on optimizing health. Systems medicine pioneers propose the creation of personal "dense, dynamic data clouds" by collecting multiple (billions) data points from each individual, and analyzing these data for any evidence of disease or disease risk.
The overall goal is to improve healthcare and health by moving from a system that reacts to diseases in a generic way to an approach that is "predictive, preventive, personalized and participatory".
PM and SM have generated global excitement. The European Union established the European Alliance for Personalized Medicine in 2012 with the aim to accelerate the development, delivery, and uptake of personalized healthcare. The same year, the UK founded the National Phenome Centre as a premier source for metabolic phenotyping. In the US, the National Institutes of Health is leading a national, large-scale PM study, called All of Us Research Program, which aims to "engage one million or more volunteers living in the US to contribute their health data over many years to improve health outcomes, fuel the development of new treatments for disease, and catalyze a new era of data-based and more precise preventive care and medical treatment." In addition, many US universities and public and private research centers have developed their own PM or SM research programs and studies.

PM and SM face challenges. Both rely on the gathering and sharing of personal data from large numbers of patients and healthy people. This raises potential privacy and discrimination issues. Another obstacle is the development of fast computing and other technologies needed to facilitate the analysis and interpretation of huge volumes of data and which can be scaled as projects evolve from pilot studies to include virtually all of the population. A third challenge, which pertains to all biomedical research endeavors, is the need to develop better biological models of disease to identify modifiable targets. These approaches require educating the general population so that they are empowered to make good decisions for their health. Finally, future medical professionals will need to be trained to have the new skills needed for PM and SM. As Leroy Hood, (a winner of the 1987 Albert Lasker Basic Medical Research Award, who spoke to us for this issue of the Lasker newsletter) noted in his interview:
"…one of the big challenges is going to be education. If you really want to have a 21st-century medical school, you want to start with your freshman class."
PM and SM are new ways of thinking about improving the health of all. They have the potential of increasing the effectiveness of therapies and reducing unnecessary side effects. They may even have the potential to prevent disease or stop its progression early on. But if we are to achieve this new vision for more patients and develop effective, tailored interventions for more diseases, sustained investment in biomedical research will be key.
