Millions of people who have undergone lab tests over the last 60 years are fortunate that Rosalyn Yalow ignored her parents’ career advice. As a college student in the 1930s, Yalow had her heart set on becoming a physicist, a profession almost no women entered then. Her parents, whom she viewed as “more practical,” urged her to follow the conventional route for intelligent young women and become a schoolteacher.

“The most rewarding satisfaction is the pleasure and excitement of having learned something that no one knew before,” said Yalow.
Credit: National Library of Medicine
But Yalow, who described herself as a “stubborn, determined child,” refused to abandon her ambition. She became the first woman in more than 20 years to be admitted to the engineering program at the University of Illinois, where she finished a PhD in physics. A little over a decade later, she and a collaborator devised a revolutionary lab technique, radioimmunoassay, which allowed doctors and researchers to measure small quantities of important molecules in the body, including hormones and drugs. “It was the first technology for reliably quantifying compounds in biological samples such as blood,” says Thomas Annesley, an emeritus professor of clinical chemistry at the University of Michigan. Radioimmunoassay became one of the most-performed medical tests. The number of people who have benefited from the technique is “in the hundreds of millions,” Annesley says. Yalow’s achievement garnered her the Albert Lasker Award for Basic Medical Research in 1976 and the Nobel Prize in physiology or medicine a year later.
Breaking into the Boys’ Club
Born in New York City in 1921, Yalow came from a Jewish family that prized education. Although neither of her parents finished high school, “there was never a doubt that their two children would make it through college,” Yalow recalled in her autobiography. Initially entranced by mathematics, Yalow entered Hunter College in New York City, intending to become a chemist, but her teachers won her over to physics. At the time it “was the most exciting field in the world,” she remembered.

Rosalyn Yalow at the Bronx Veterans Administration Hospital, October 13, 1977
Credit: US Information Agency
After finishing her degree in 1941, Yalow tried to continue her physics studies, but every graduate school she applied to turned her down. Other scientists who knew and worked with Yalow say that her being female and the pervasive anti-Semitism of the time were likely factors in the rejections. Undeterred, Yalow found what she called a possible “back door” into research: becoming a secretary for a biochemist at Columbia University in New York City. The job might eventually allow her to shift to lab work, but she would need to learn shorthand. Only a month after she started a secretarial class, a school that had initially turned her down, the University of Illinois, offered her a graduate position in physics and a stipend. One of her Hunter College teachers had persuaded the school to take a chance on her. “I tore up my stenography books,” Yalow recalled, and shortly afterward left New York City for the only extended period in her life.
During her 3½ years at the University of Illinois, “I was no longer a stubborn, determined child but rather a stubborn, determined graduate student,” Yalow wrote. She excelled by outworking her fellow students, according to her biographer, Eugene Straus. He notes that she often slept in the bathroom at the lab so she could keep experiments going late into the night. She also performed well academically, although the chairman of the physics department told her that the A- she received in the optics lab course “confirms that women do not do well at laboratory work.” Yalow shrugged off his comment.

Yalow in the laboratory (1970s)
Credit: National Library of Science
Harder to shrug off were her lack of job offers after graduation. With no academic opportunities, she finally got hired as an engineer at a US government lab. A year later, she moved back to Hunter College to teach physics. But she wanted more. Although she was teaching full time and trying to start a new home with her husband, those obligations “were hardly enough to occupy my time fully,” she wrote. Yalow began performing unpaid research in a Columbia lab studying the medical uses of radioactivity. She impressed the scientists there, who spread the word about her talents. Soon Yalow had a new job as a medical physicist at the Bronx Veterans Administration (VA) Hospital in New York City, where she spent the rest of her career.
Going Nuclear
In the late 1940s when Yalow started at the VA, doctors had just begun to explore the benefits of radioactive isotopes for treatment and diagnosis. Yalow knew the physics of radioactivity but didn’t have a medical background, so she began hunting for a collaborator to fill that gap. When she met Solomon Berson, an MD also working at the hospital, she found her scientific soulmate. Like her, he was an outsider who had persevered through rejection—more than 100 medical schools spurned him before he got into New York University. Their scientific partnership began in 1950 and lasted almost 20 years.
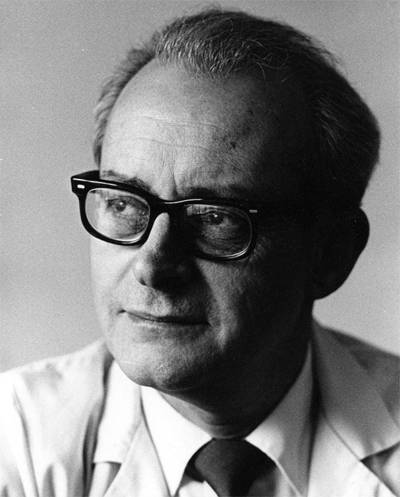
Solomon Berson
Credit: The Arthur H. Aufses, Jr. MD Archives, Icahn School of Medicine at Mount Sinai/Mount Sinai Health System, New York, N.Y.
Straus, a physician who performed research with Yalow and Berson, likens the atmosphere in their lab to an intellectual tennis match in which “concepts and approaches to problems flew between them.” Yalow and Berson were “very different people,” and as a result they complemented each other, says Shimon Glick, an emeritus professor of medicine at Ben-Gurion University of the Negev in Israel who worked with the pair for three years in the early 1960s. Berson, Glick says, “was the smartest person I ever met.” He also was volatile, and his thinking could get bogged down in complex mathematics. Yalow, by contrast, was more grounded. “She was the steadying factor in the lab,” Glick says.
Yalow and Berson started their collaboration by using radioactive isotopes to measure several physiological variables. For instance, one of their first achievements was to refine the technique for determining the volume of blood in a patient’s body, an important measure that can change in illnesses such as heart failure and kidney disease.
Radioimmunoassay grew out of their interest in insulin, the hormone that spurs cells to absorb glucose from the blood. Researchers at the time wanted to figure out why patients with type II diabetes had high blood sugar levels despite producing ample insulin. Another scientist had hypothesized that an enzyme must be rapidly breaking down the insulin before it could decrease blood sugar.
To test that idea, Yalow and Berson injected insulin tagged with radioactive iodine into a group of research subjects, some of whom had diabetes. By collecting blood samples at different times after the injections and measuring the amount of radioactive iodine, the pair could gauge how long insulin lingered in the blood. Their data showed that the enzyme hypothesis was wrong—researchers now know that in type II diabetes, cells lose their sensitivity to insulin.

Yalow and Berson shared 22 years of scientific discovery and adventure.
Credit: The Arthur H. Aufses, Jr. MD Archives, Icahn School of Medicine at Mount Sinai/Mount Sinai Health System, New York, N.Y.
That work shows the pair’s scientific acumen. As Glick notes, other researchers had tested the enzyme hypothesis in that way, but Yalow and Berson noticed something everyone else missed: The results depended on whether subjects had received insulin injections before. In patients treated with insulin for a long time, the hormone disappeared from the blood more slowly than in patients who hadn’t previously received injections or had just begun to get them.
Radioimmunoassay Is Born
That observation proved momentous because it suggested to Yalow and Berson that some molecule was latching onto the insulin and keeping it in the blood. Further experiments revealed the molecule was an antibody, one of the body’s defensive proteins. In the 1950s, medical insulin came from slaughterhouse animals, and the immune system recognized the molecule as foreign. But the body takes time to start producing antibodies against animal insulin, which explains why only patients who had previously received the hormone carried those antibodies at the beginning of the study.
When Yalow and Berson sent their findings to a leading scientific publication, “the journal said no way, it cannot be,” Glick says. Insulin is a tiny protein, and at the time researchers were certain that antibodies could grab onto only heftier molecules. After plenty of wrangling, in 1956 the journal’s editor agreed to publish the paper, but with one proviso: Yalow and Berson had to remove the word “antibody” from the title.
The researchers realized that their results served as the basis for a new technique to measure substances in the body. Four years later, they publicly unveiled radioimmunoassay. The technique relies on antibodies to recognize the molecule of interest. Measuring a patient’s insulin levels, for instance, involves mixing a blood sample with antibodies that bind to insulin. Another essential ingredient is radioactively labeled insulin, which competes with insulin from the patient’s blood to attach to antibodies. After the antibodies and their captured insulin are removed, the leftover radioactivity indicates the insulin concentration in the patient’s sample. The greater the concentration of insulin, the more radioactive insulin it displaces from the antibodies.
“They were quite a ways ahead of everyone,” Annesley says. Radioimmunoassay outperformed methods available in the early 1960s, such as standard pregnancy tests, which involved injecting urine from the would-be mother into a frog or rabbit. Unlike those nonquantitative tests, radioimmunoassay can measure the amount of human chorionic gonadotropin, a hormone the placenta makes during pregnancy, in a sample. Radioimmunoassay also is sensitive. Those virtues made it the go-to method for detecting hormones, vitamins, drugs, tumor proteins, and other molecules, as well as for screening blood for the presence of viruses. Some early pregnancy tests also were based on the technique. Radioimmunoassay also was a boon for physiologists probing how the body functions, allowing them to measure and track key variables, Glick says. “It changed the whole field.”
Carving Out Time for Family
Glick recalls that Yalow worked extremely long hours, arriving at the lab early and staying late. Even with her other responsibilities, including her husband and two children, she took good care of what she called her professional family, the researchers like Glick who worked in her lab. She was protective, Glick recalls, and would intervene if anyone attacked the lab members’ work in print or at conferences. “She was like a lioness with her cubs,” he says.
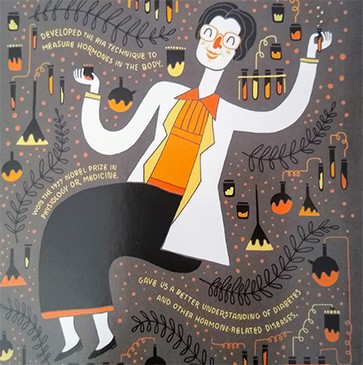
Detail of a postcard honoring Yalow
Credit: Whoisjohngalt
Yalow and Berson’s partnership broke up in 1968 when he left to run a department at the Mount Sinai hospital. He died four years later, leaving Yalow to continue probing the roles of insulin and other hormones. Researchers in her field agreed that the development of radioimmunoassay was worthy of major scientific awards. However, her peers weren’t sure whether a woman would receive such distinctions when her male collaborator had died. But in 1976, Yalow became the first woman to win the Albert Lasker Basic Medical Science Award. In 1977, she shared the Nobel Prize with two male recipients who had worked on unrelated research.
Yalow retired from the VA in 1992 and died in 2011. Her brainchild remains a staple of medical care and research. Radioimmunoassay is still the standard for measuring levels of a protein that appears in the blood after a heart attack, for instance. However, many medical tests in use today have abandoned radioactive isotopes in favor of safer means of detection, such as fluorescent molecules. Still, Annesley says, “they use the same principle of antibody binding” that Yalow first harnessed almost 70 years ago.
By Mitchell Leslie

