On a cold, snowy Saturday afternoon in February 1933, a farmer drove onto the University of Wisconsin campus in Madison with a dead cow, a milk can of blood, and 45 kilograms of sweet clover hay. Several of his cows had bled to death, and he had traveled more than 200 kilometers in the hope that the state veterinarian could help him save the herd's other ill members. But the veterinarian's office was closed. Instead, the farmer met with biochemist Karl Link, whose lab had just started studying sweet clover.
Although not a veterinarian, Link realized that the farmer's animals suffered from sweet clover disease, a recently discovered and often fatal condition caused by moldy hay. Link wrote that he advised the farmer "to stop feeding that hay, and possibly transfuse those desperately sick cattle." But because nobody knew the chemical basis of the disease, Link could offer no help beyond that. He told the farmer that "eventually it might become possible to make some usable recommendations to avoid such disasters, but not now."
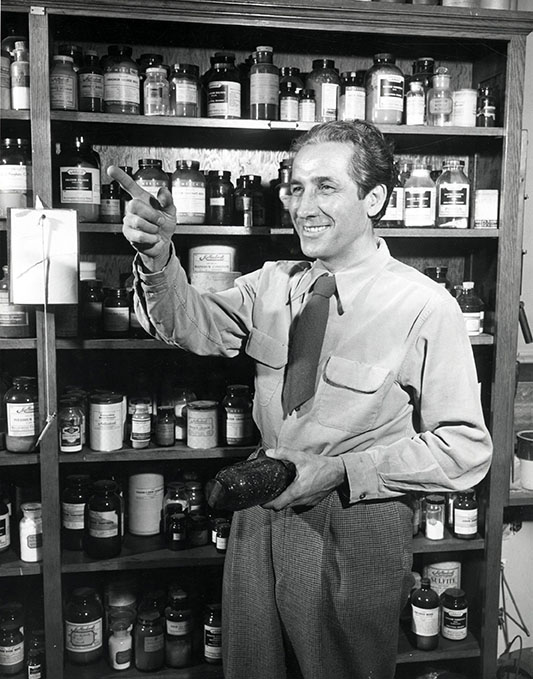
Karl Paul Link in front of a cabinet of chemicals (1950)
Courtesy of Board of Regents of the University of Wisconsin System
The farmer's visit served as "a direct catalytic hit," spurring Link to investigate why spoiled sweet clover caused animals' blood to stop clotting. The payoff from more than a decade of research by Link and his students went far beyond animal husbandry. They developed the anticoagulant warfarin, the first widely used treatment for people with blood clots or who are susceptible to them, including patients with atrial fibrillation, deep vein thrombosis, pulmonary embolism, or replacement heart valves. "Warfarin was for 65 years or more the only oral blood-thinning agent we had," says hematologist Jeffrey Weitz, executive director of the Thrombosis and Atherosclerosis Research Institute in Canada and professor of medicine at McMaster University.
Link's achievement made him one of only a few researchers to win two Lasker Awards. He took home the Albert Lasker Basic Medical Research Award in 1955 and shared the Albert Lasker Clinical Medical Research Award in 1960. "He's probably saved more lives than the average biochemist will ever conceive of doing," says Jerold Last, a biochemist at the University of California Davis Medical Center.
But Link's influence extends even further because warfarin sparked the development of a new generation of oral blood thinners, such as apixaban (Eliquis) and rivaroxaban (Xarelto), that block clotting through different mechanisms and are easier and safer for patients to take. "If you look at the evolution of the field, he had a huge impact," Last says. The irony, he adds, is that if Link had followed his original plan, warfarin would have been only a rodent poison.
Link, an extrovert and extravagant dresser who might come to his lab wearing a cape he picked up during his postdoctoral work in Switzerland, stood out on campus. "When he walked into a room, everybody knew he was there," says Last, who was a graduate student at the University of Wisconsin late in Link's career. But Link also was a top-notch scientist adept at microchemistry, the analysis of minute amounts of substances. "Link's microchemical lab was a showplace," a former student recalled. He boasted the know-how and equipment necessary to identify the culprit in sweet clover disease.
Despite Link's expertise, he and his students had to navigate "a long and arduous trail" to isolate the chemical, he wrote. The researchers quickly ran into a problem: the lack of a standard test to measure whether a compound inhibited blood clotting. "The immediate prospects of developing a reliable and simple bioassay were not bright," he wrote. "We had not had previous experience with that complex problem—blood coagulation." More than four years after the farmer's visit, he and his colleagues devised a suitable test, which relied on diluted rabbit blood.

Karl Paul Link (right) performs a laboratory procedure with fellow researcher Mark A. Stahmann (1940). Together they discovered dicumarol, a powerful anticoagulant.
Courtesy of Board of Regents of the University of Wisconsin System
When Link and his students began analyzing the chemical composition of sweet clover, they discovered that the plants were "a kind of biochemical grab-bag," teeming with molecules that might affect clotting. As the team systematically evaluated the compounds with the blood assay, several were initially promising but didn't pan out. Or, as Link put it in his flamboyant style, "many a seething and simmering hope did not become reality." More than six years after the farmer's visit, Link's student Harold Campbell finally purified 6 milligrams of the anticlotting compound, which the researchers named dicumarol. They discovered that dicumarol formed from another chemical when sweet clover hay began to spoil. They then "turned dicumarol over to the clinicians," Link recalled.
Doctors could already prescribe one anticoagulant, heparin, that researchers had first isolated from a dog's liver nearly 30 years before. But the drug was expensive and had to be injected or given by infusion. Dicumarol, by contrast, was a pill. Starting in the early 1940s, the other two recipients of the 1960 Lasker Award—Edgar Allen of the Mayo Clinic and Irving Wright of what was then Cornell University Medical College—helped pioneer dicumarol treatment for a variety of conditions. Between them, they tested the drug in thousands of patients, showing its value for preventing blood clots after surgery and in other situations.
Although the drug offered some advantages over heparin, both drugs suffered from "deficiencies which make desirable a continued search for an ideal anticoagulant for clinical use," Allen wrote in 1947. Team Link was already on the case. The scientists synthesized more than 100 variants of dicumarol and began gauging each one's clot-blocking capabilities. Number 42 on the list combined two important qualities: it was more potent than dicumarol but didn't seem to cause excessive bleeding. Link named the molecule warfarin after the Wisconsin Alumni Research Foundation, which underwrote some of the lab work.

Warfarin, molecular model, carbon (grey), hydrogen (white) and oxygen (red)
Courtesy of Laguna Design / Science Source
Link's next decision "shook the laboratory," as he put it. He declared that the new compound was suitable only for killing rats and mice, not treating patients. That choice may seem baffling, but it reflected Link's mistrust of the medical profession, Last says. At the time, the biochemistry building where Link worked was on the opposite side of the campus from the medical school, and that physical separation reflected the intellectual gulf between the two disciplines, Last says. "Link was quite certain that the average physician would not really understand the critical doses that would be helpful rather than unhelpful."
As a result, the most prescribed anticoagulant of all time first hit the market in 1948 as a product for rodent control.
In 1951, however, a soldier in Pennsylvania tried to kill himself by eating a package of warfarin. He survived. "This incident acted as a catalyst," Link wrote, helping convince him that warfarin could be a safe drug. Doctors began studying warfarin in patients, leading the Food and Drug Administration to approve it as a treatment in 1954. Warfarin still faced competition from heparin and other anticoagulants but got a big boost the next year when President Dwight Eisenhower's doctors gave him the drug after a heart attack, Last notes.
Warfarin has been a staple of anticoagulation treatment ever since. "Some patients do very well" on the drug, says hematologist Sam Schulman, director of the Thrombosis Service at HHS-General Hospital in Hamilton, Canada, and a professor of medicine at McMaster University. He has recommended it so many times in his nearly 50-year medical career that "I'm known as the biggest prescriber of warfarin in Ontario."
Still, warfarin has significant drawbacks. It's less convenient than most other oral medications. "You have to tailor the dosing regimen for each person," Weitz says. When patients start taking the drug, they must travel to an anticoagulant clinic twice a week for clotting tests. Those visits become less frequent as doctors identify the optimal dose. But patients still require regular monitoring, which typically means returning to the clinic every month, Weitz says.
Patients also must watch what they eat because certain foods alter the drug's effectiveness. In addition, warfarin can interact with 650 other medications, including many antibiotics, ibuprofen, and acetaminophen. The drug also can trigger excessive bleeding. Warfarin was once the prescription drug most likely to send a patient to the emergency room.
Those downsides spurred pharmaceutical companies to develop a family of drugs known as direct oral anticoagulants, which include apixaban, rivaroxaban, edoxaban (Lixiana, Savaysa), and dabigatran (Pradaxa). Warfarin works by slashing levels of vitamin K, which is essential for synthesizing several key proteins involved in clot formation. Direct oral anticoagulants, however, rely on a different mechanism, targeting either of two proteins that help orchestrate clotting: factor Xa or thrombin.
The newer drugs, which first reached the market in 2010, outperform warfarin in several ways. For example, they halve the risk of intracranial bleeding, a potential side effect of anticoagulant treatment, Schulman says. The main benefit, however, is that patients do not need regular clotting tests. As a result, the medications "are convenient for the patient and for family doctors," he says. That advantage shows up in the number of prescriptions. Between 2013 and 2022, the number of people in the United States taking warfarin declined from nearly 5 million to 1.6 million.
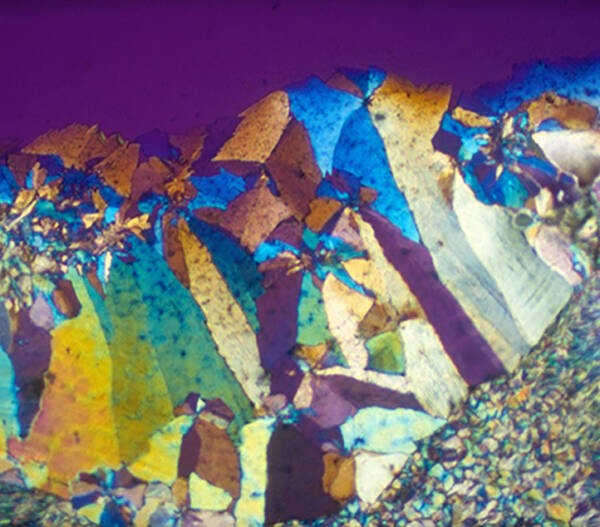
Polarized light micrograph of warfarin crystals
Courtesy of Leonard Lessin / Science Source
Despite those advances, "there are still patients [for whom] we need warfarin," Weitz says. It's the only anticoagulant that some patients can take, including those with mechanical heart valves or who have the autoimmune disorder antiphospholipid syndrome. Warfarin's low cost also makes it the anticoagulant of choice in many poorer countries, Schulman says. Research also has identified a surprising upside to the anticoagulant clinic requirement, he notes. Many patients who need warfarin are elderly, and some begin to look forward to the visits as opportunities to get out of the house and catch up with friends, he says. "It was almost like a social benefit for them."
Researchers are now testing the next generation of anticlotting treatments, known as factor XI inhibitors. Some of those drugs are antibodies that lock up factor XI, an essential protein in the series of responses that induces clotting. Other inhibitors under study include antisense oligonucleotides, short relatives of DNA and RNA that cut cells' production of factor XI, and small molecules that inhibit factor XI activity. Although the new drugs draw on a deeper understanding of blood clotting mechanisms than Link and his peers had, he set the stage for their development when he decided to pursue the cause of sweet clover disease in 1933. "Karl would be astounded at how we have moved past warfarin," Weitz says.
By Mitchell Leslie