In the 1960s, patients with cancer in New York’s Harlem community, which was then poor and predominantly African American, were dying much faster than patients in most other parts of the country. On average, only 39% of Harlem women with breast cancer lived for five years, well below the national average of more than 75%.
When Harold Freeman walked into Harlem Hospital Center as its new attending surgeon in 1967, he was confident that he could turn the bleak mortality figures around. Freeman, who had just completed his surgical training at Memorial Sloan Kettering Cancer Center, wrote “I imagined that I could ‘cut cancer out of Harlem'”.
“It was sobering for me that I couldn’t do that,” Freeman recalls. The problem proved to be much more difficult than he had anticipated. As he quickly discovered, Harlem’s high cancer death rate reflected deeper social and economic factors that he would have to confront. “You can’t cut cancer out unless you deal with what’s happening in the community,” he realized.
Left to right: Freeman with board members Dan Koshland and James Fordyce at the 2000 Lasker luncheon
The approaches that Freeman introduced in the next few decades dramatically reduced cancer mortality in Harlem and transformed how patients throughout the country interact with the healthcare system. His efforts earned him a Lasker Award in 2000, which cited his commitment to “ensure that all people receive the best possible care, regardless of their color or income.”
From the beginning, the Lasker Awards have honored not only researchers who made important basic or clinical research discoveries but also organizations and individuals like Freeman who help deliver the benefits of scientific and healthcare advances to people who need them most. The first two recipients of the Lasker Public Service Award in 1946 were Fred Soper of the Rockefeller Foundation, who led battles against yellow fever and malaria in Brazil and other countries, and Alfred Richards of the University of Pennsylvania, who propelled the mass production of penicillin during World War II. Today, the Lasker~Bloomberg Public Service Award recognizes four categories of achievements: funding research or public health efforts; improving public understanding; serving as a spokesperson for medical research or public health; and providing outstanding public health practice.
Steering Patients with Cancer Toward Better Outcomes
Before Freeman could reduce cancer mortality among his patients at Harlem Hospital Center, he had to determine why their death rate was so high. He found that many of his patients with breast cancer had not sought medical care until they had advanced disease and it was “too late.” In some cases, their tumors had grown into “ulcerated masses” that could not be removed, he says. “I hadn’t seen anything like that.” When he interviewed some of the patients, however, they explained that they had tried to obtain treatment, but the healthcare system had thwarted them. For example, some had gone to the emergency room when they discovered their cancers, only to be told that a breast tumor was not an emergency.
One of the first solutions he tried was to launch Harlem’s first free breast cancer screening clinic, which is still open today. But he recognized he had to do more because the complexity of the healthcare system created numerous barriers for the poor. To overcome these obstacles, he ‘invented’ a new type of healthcare specialist, the patient navigator. A navigator shepherds individuals through the often-labyrinthine process of obtaining medical care, assisting with every step of diagnosis, treatment, and recovery. The tasks a navigator might perform include helping patients to obtain insurance, ensuring that they keep their appointments, arranging for childcare, and helping them communicate with their doctors.
These actions made an impact. “We increased five-year survival from 39% to 70%” among patients with breast cancer in Harlem, Freeman says. His introduction of patient navigators had an even bigger effect. They have become standard for patients with cancer — and a variety of other diseases — at hospitals throughout the United States and in other countries.
Superman’s Surprising Superpower: Public Advocacy
Graduation ceremonies at the University of Virginia are usually raucous, and the celebrating students typically do not pay much attention to the speakers, says Oswald Steward, who was a neuroscience professor at the school for 25 years. But the 1998 commencement was different, Steward recalls. The speaker, actor Christopher Reeve, transfixed the audience of 4000 to 5000 by describing his life after he was paralyzed from the shoulders down. “During his speech there was perfect silence,” says Steward. “He didn’t ask for quiet. It was his power” that quieted the crowd.
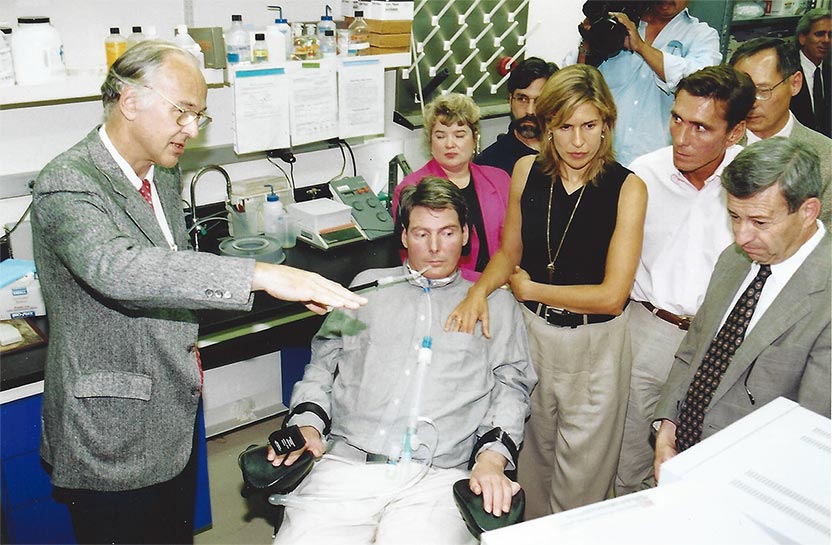
Chris and Dana Reeve visited University of Califronia, Irvine (UCI) research labs (1996).
Image courtesy of UCI Communications
Reeve, who won a Lasker Award in 2003, became an important advocate for research on spinal cord injuries because he could seize the attention of not just restive college students but also members of Congress, philanthropists, researchers, the press, and the public.
After playing Superman in four movies in the 1970s and 1980s, Reeve suffered two fractured neck vertebrae in 1995 when a horse threw him during an equestrian event. Before his accident, “people didn’t think much about spinal cord injury. Then suddenly this person, literally Superman, suffers a devastating spinal cord injury,” says Steward, who now heads the Reeve-Irvine Research Center at the University of California, Irvine. Convinced he had to do something to help other patients with similar injuries, Reeve capitalized on his celebrity and compelling personal story. He gave numerous interviews, testified in favor of increased National Institutes of Health (NIH) funding before Congress, opened the Democratic Convention in 1996, and argued for stem cell research.
From the beginning, Steward says, Reeve realized that good science is crucial to improving the lives of people with spinal cord injuries, and promoting research was one of his goals. The organization that he and his wife, Dana, launched in 1996, now known as the Christopher & Dana Reeve Foundation, continues to fund investigations into new treatments and has provided $26 million in quality-of-life grants for organizations aiming to improve conditions for patients with paralysis. Reeve’s interview with Barbara Walters in 1995 sparked the creation of the Reeve-Irvine Research Center, where scientists probe how to repair the spinal cord and restore function in patients. Reeve died in 2004, but “he had an immense influence” during his life, says Steward.
Dear Ann Landers . . . I Have a Problem with the US Senate
A 1985 Lasker Award winner, Eppie Lederer, better known as the advice columnist Ann Landers, wielded her clout with millions of newspaper readers to prod Congress to pass the National Cancer Act, a 1971 law that bolstered cancer research in the United States.

Eppie Lederer, also known as Ann Landers
In a syndicated column that ran for 47 years, Lederer counseled disgruntled spouses, fed-up parents, heartbroken lovers, and other wisdom-seekers. Then one day in February of 1971, she heard from her friend Mary Lasker. Lasker had been pushing for more cancer research funding since the 1940s, and in the late 1960s she and her allies began campaigning for a crash program to cure the disease, a cancer ‘moon shot’ analogous to the Apollo program. At the time, they argued, science was not delivering new treatments fast enough, but with a big enough boost, researchers could uncover a cure.
In the spring of 1971, the Senate was considering a bill that would furnish that boost by dramatically increasing the budget of the National Cancer Institute (NCI). Another provision of the bill would set up the NCI as a separate agency independent of the NIH, creating the cancer equivalent of NASA that would make the disease a priority. But the bill’s prospects looked grim. The NIH opposed it. The NCI opposed it. The American Medical Association opposed it. The bill even drew flak from some researchers, who asserted that scientists did not know enough about cancer to allocate the extra money intelligently.
Lasker decided to enlist the public to win over reluctant senators, and she asked Lederer to help. In her column on April 20, 1971, Lederer told readers, “Today, you have the opportunity to be part of the biggest offensive against a single disease in the history of our country.” She urged them to write to their senators, “or better yet, send telegrams,” in support of the bill. Readers responded, dispatching about one million letters to Congress, the most received until that time about any issue. Senators took heed and passed the bill in June.

President Richard Nixon signing the National Cancer Act on December 23, 1971
Image courtesy of the National Cancer Institute
The final National Cancer Act that President Nixon signed in December of 1971 did not include some of the measures that Lasker and her allies sought. It did not detach the NCI from the NIH, for instance. But the act did increase the NCI’s clout and independence by giving the agency control over its own budget and making its director a presidential appointee. In addition, the law more than tripled the NCI’s budget over three years. The National Cancer Act’s legacy also includes funding for a network of cancer research centers, such as the Fred Hutchinson Cancer Research Center, that today are hotbeds of scientific investigation and provide the latest treatments.
Slashing Vaccine Costs to Save Poor Children
A 2019 Lasker Award winner, Gavi, the Vaccine Alliance, is estimated to have saved the lives of as many as 13 million children. The organization has provided vaccinations to more than 760 million children since it was founded in 2000. At the time, public health experts realized that other international vaccine efforts were losing steam. Around 30 million children in developing countries had not received all of the vaccines that kids in richer nations typically received, mainly because of the high cost of new immunizations. “A market failure” put these vaccines out of the reach of the developing countries, says Seth Berkley, Gavi’s CEO. To correct this failure, a group of partners that included the Bill & Melinda Gates Foundation, the World Health Organization (WHO), UNICEF, the governments of developing countries, and vaccine manufacturers teamed up to launch Gavi. “Gavi was created to pool demand from 73 developing countries, home to 60% of the world’s children, to drive down the cost of vaccines while boosting supply for these countries,” says Berkley.

Seth Berkley delivers rotavirus vaccine in Ghana.
This new approach paid off. Today, countries supported by Gavi can provide a child with the 11 vaccinations recommended by the WHO for $28, whereas the same immunizations cost $1100 in the United States. Gavi has used novel strategies to ensure that vaccines are affordable and available. One example is the financing arrangement that sped deployment of vaccines against pneumococcal diseases, which kill more than 500,000 children every year. About a decade ago, the United States and Europe introduced upgraded vaccines that protect against these diseases, but new vaccines can take 10 years or more to reach developing countries. To motivate pharmaceutical companies to furnish these vaccines to poorer countries, Gavi and its partners pioneered an approach called an advance market commitment, in which donors provide subsidies to manufacturers that commit to supply the vaccines at a set price for a certain time. Two companies, GlaxoSmithKline and Pfizer, initially agreed, and as a result, developing countries were giving the new pneumococcal vaccines just a few months after their introduction in the developed world.

A nurse administers pneumococcal vaccine.
Gavi also accelerated development of the first approved Ebola vaccine. Although researchers have been investigating how to create vaccines against the disease for more than 20 years, manufacturers were reluctant to take any candidates through the expensive process of licensing or gaining approval from regulators, Berkley notes. But after the 2014 Ebola epidemic in West Africa, Gavi made manufacturers an offer. “Gavi would make a legal commitment to buy millions of dollars’ worth of doses of a licensed Ebola vaccine if a manufacturer would commit to taking it through the licensing process as well as making a stockpile of investigational doses available,” Berkley says. One manufacturer, Merck, agreed, and its Ebola vaccine received approval in 2019 after only five years, “half the time of a standard vaccine,” says Berkley. Moreover, he adds, the supply of investigational doses proved invaluable for fighting two Ebola outbreaks in the Democratic Republic of the Congo that began in 2018.
All of these winners made a large impact on public health. But some say that winning the Award also made an impact on them. Freeman, for example, held many important positions, including director of surgery at Harlem Hospital Center, president of the American Cancer Society, and associate director of the NCI. But he says that receiving a Lasker Award stands out in his career because it “gave me more strength, more visibility, and more respect.”
by Mitchell Leslie