The CZU Lightning Complex wildfire that charged through California's Santa Cruz mountains in August and September of 2020 was ravenous. The blaze, the subject of a new film produced by iBiology and sponsored by the Lasker Foundation, destroyed nearly 1500 buildings and devastated thousands of hectares of land, much of it old-growth redwood forest. The fire itself killed only one person. However, the people who lived through the blaze, including the 70,000 residents who had to temporarily evacuate, could suffer its consequences for years to come.

Sparked by lightning, the CZU Lightning Complex fire torched 35,000 hectares in California's Santa Cruz mountains.
Courtesy of Pierre Markuse, Germany
Along with the obvious injuries — burns during fires, broken limbs during earthquakes — natural disasters spur a variety of short-term and long-term effects on physical and mental health. They harm the heart, lungs, and immune system. They take the lives of people who are far from their path and derail the development of unborn children. They deliver psychological blows that can be as devastating as those resulting from combat and mass shootings. "The mental health effects impact more people across a broader geographical area and over a longer span of time than do the physical effects," says psychiatrist Joshua Morganstein of the Uniformed Services University in Bethesda, Maryland. And because disasters are becoming more common and more severe, the number of people who will face these repercussions in the future is rising.
A Breath of Foul Air
The fire that charred the Santa Cruz redwoods was just one of more than 100 wildfires that burned across the western United States in 2020. They transformed more than 3 million hectares of trees, brush, and buildings into dense smoke that shrouded much of the West, including major cities such as San Francisco and Portland.
Breathing this smoke "can be immediately and acutely harmful to human health," says Sarah Henderson, senior environmental health scientist at the British Columbia Centre for Disease Control in Canada. Wildfire smoke is a complex brew of noxious and toxic chemicals, including formaldehyde, carbon monoxide, ozone, and nitrogen dioxide. But its most dangerous ingredient may be the fine particles known as PM2.5. Because these particles are so small, breathing can suck them deep into the lungs. They can even slip into the bloodstream. The immune system attacks PM2.5 as if it were an invading bacterium or virus but cannot eliminate it, says Henderson, leading to systemic inflammation that can irritate and damage the lungs and other organs.

Santiago Fire, California, 2007
The fires triggered the largest evacuation in county history (more than 500,000 people).
Courtesy of Bighead
Because people with respiratory illnesses are more susceptible to smoke, wildfires typically trigger a surge in breathing problems, sending many of these people to the hospital. In 2007, for example, large wildfires burned across 13% of San Diego County in California. One study of county medical records found that emergency room visits for asthma shot up 112% when the air quality was at its worst.
Another possible outcome of breathing wildfire smoke is death. "We see a small but significant increase in mortality when it's smoky," says Henderson. Researchers still need to work out who is at risk of dying, Henderson notes, but the toll can be high. Scientists at Stanford University estimated that more than 1200 people in California died because of smoke from the 2020 fires, whereas the flames killed 26. And globally, smoke from landscape fires — which include wildfires and blazes that are intentionally set to clear land for agriculture — is responsible for more than 340,000 deaths every year, Henderson and her colleagues have calculated.
Most people who breathe wildfire smoke don't die immediately, of course, but they could incur long-term damage to their health. Researchers have linked prolonged exposure to other types of air pollution to chronic obstructive pulmonary disorder (COPD), heart disease, asthma, lung cancer, and other diseases. We are continually inhaling pollutants, however, so ascribing specific illnesses to wildfire smoke has proven difficult. Whether it raises the odds of developing lung cancer, for example, is unknown. "It's one of many risk factors that go into how healthy you are throughout your life," says Henderson.
Research does point to long-term impacts for fetuses and infants. One striking study tracked the health of monkeys living in an outdoor facility at the University of California, Davis. For two months in 2008, smoke emanating from several fires veiled the area. Scientists later discovered that monkeys that were babies at the time had weaker immune systems and 20% smaller lungs than did monkeys that were born when the air was cleaner. The results jibe with findings that indicate 'ordinary' air pollution impairs lung development in children.
Heartbroken
Natural disasters deliver a jolt to the cardiovascular system. In the first days after an event, hospitals typically see a spike in heart attacks. But the baleful effects can last much longer, cardiologist Anand Irimpen of the Tulane Medical Center in New Orleans and his colleagues have discovered. Irimpen and his family evacuated to Dallas when Hurricane Katrina hit Louisiana in August of 2005. When they returned to New Orleans the following February and Irimpen restarted his job at the medical center, his colleagues told him that their workload was heavier because so many patients were suffering heart attacks, he recalls. At first, he was skeptical, but eventually, he and his colleagues decided to perform a study.

Hurricane Katrina damaged or destroyed about 70% of the homes in New Orleans.
Courtesy of David Shankbone
For their first analysis, published in 2009, the researchers tallied the number of patients admitted to the hospital for heart attacks in the 2 years preceding Katrina and in the 2 years after the storm. "We found a threefold increase in heart attacks after Katrina," says Irimpen. "I was taken aback." Even more surprising was how long the increase has persisted. The most recent data, which Irimpen and colleagues presented at a scientific conference in 2020, suggest that the rate is now four times higher than before the hurricane.
The disaster also shifted the timing of heart attacks, Irimpen and his team found. Heart attacks tend to occur early in the day during the work week — Monday morning is the peak time. But the Katrina survivors were arriving at the hospital in the evening and on weekends.
The researchers aren't sure why the incidence of heart attacks soared after the hurricane, but they do have a prime suspect. "We feel that stress is a key factor that causes the increase in heart attacks in these patients," says Irimpen. That hypothesis could help explain why the effect has lingered for so long. Recovery from the hurricane was protracted. Many people were out of work for long periods, and rebuilding and repair often took years. Stress could also be the reason for the altered timing of heart attacks. Home typically provides a refuge from the pressures of the day, but for Katrina survivors it was a source of stress, forcing them to confront the difficulties of restoring their lives, says Irimpen. Thus, they were more likely to have heart attacks after hours.
Irimpen adds that stress is not the only possible contributor to the heart attack spike. The hurricane disrupted people's lives in many ways that could undermine cardiovascular health. Getting exercise was more difficult because gyms were closed, for example, and many people lost or stopped taking their medications. Because residents were out of their homes and could not cook for themselves, they found it harder to eat a healthy diet, he says.
A Mental Health Blow — For Some
Disasters are agonizing for survivors. They may barely escape death and may lose their family members, homes, and livelihoods. But nailing down the impact on mental health has been difficult because researchers usually lack the baseline data necessary to track changes in subjects' psychological condition, says gerontologist Rachel Pruchno of Rowan University in Glassboro, New Jersey.
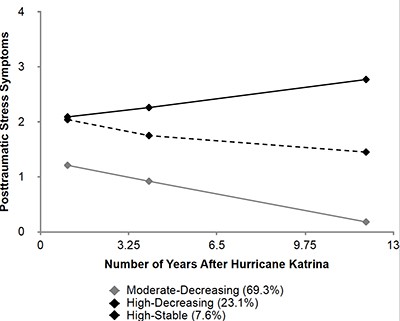
Survivors of Hurricane Katrina followed three mental health trajectories after the storm.
Courtesy of Sarah Lowe
In some cases, however, scientists have teased out insights by capitalizing on studies that were already running when a disaster occurred. Clinical psychologist Sarah Lowe of Yale School of Public Health in New Haven, Connecticut, and her colleagues redirected a survey of low-income community college students in New Orleans that started almost two years before Katrina. Their research over more than a decade has uncovered several mental health outcomes among the students. Her work and other studies indicate that only around 5% to 10% of survivors develop chronic post-traumatic stress disorder (PTSD). "Most people don't experience PTSD even when they are highly exposed" to traumatic events, she says. Instead, more than 60% of Katrina survivors showed what she and her colleagues describe as a pattern of recovery. Although they felt moderate distress shortly after the disaster, their symptoms decreased over time. For another 25%, the hurricane was more vexing; they initially had high levels of PTSD symptoms and were still showing intermediate levels 12 years later. The scientists found that a few people even thrived and managed to improve their life situations.

Floodwaters from Hurricane Sandy left parts of New York City underwater.
Courtesy of David Shankbone
Researchers have identified several factors that determine how well people cope. Pruchno and colleagues discovered that experiences during the disaster make a difference. When Hurricane Sandy hit New Jersey in 2012, the researchers were already conducting a study of healthy aging among residents of the state, allowing them to follow changes in the subjects' mental health. "People who were fearful during the disaster were the ones for whom it had the greatest impact," Pruchno says. Fear even outweighed setbacks such as losing a home.
"A lot of how people do after disasters is determined by how they did before," says Lowe. And the factor that stands out in study after study is social connectedness, or how much aid and concern survivors receive from their family and community. In a survey of workers at the Florida Department of Health who lived through hurricanes in 2004 and 2005, for instance, Morganstein and his colleagues determined that "people who live in strong communities where they feel other people are looking out for them report less PTSD and depression." Lowe's and Pruchno's studies also point to support from relatives and neighbors as key to resilience.
Inheriting Stress
Even resilient people fall victim to stress during a disaster. If they happen to be pregnant at the time, their unborn children may pay the price, developmental psychologist Suzanne King of McGill University in Montreal and colleagues have discovered. For two decades, the scientists have probed the consequences of a 1998 winter storm that knocked out electricity to parts of Quebec, Canada, for up to 40 days. Their study, Project Ice Storm, has tracked a group of about 200 children who were in the womb during the power outage.

The great ice storm of 1998, Quebec
As freezing rain falls, everything on the ground is covered in a layer of ice including power lines, roads, and trees.
Courtesy of NOAA National Weather Service
Researchers think that when a mother is under emotional pressure, stress hormones she produces traverse the placenta and enter the fetus. These molecules can disrupt the baby's physiology and metabolism and impair brain development, triggering lifelong consequences. The storm provided King and her team with an objective way to measure how much stress each mother was exposed to — how long her power was out.
She and her colleagues found that the mothers' experiences during the storm affected the physical, mental, and behavioral development of their children. Kids whose mothers were without power the longest scored lower on intelligence tests and were slower to pick up language. They got into trouble at school more often, were more anxious, and were more likely to be depressed. King and her team found that exposure to stress altered the children's DNA, changing the pattern of chemical modifications that help control which genes are switched on or off.
The children in Project Ice Storm are not doomed to dysfunction, however. Most of them come from families with above-average education and income, says King, and the reduction in intelligence she and her team measured translates into "getting A minuses instead of As." Moreover, the team discovered that mothers who were more involved with their children could alleviate some negative consequences. "Good parenting seems to be able to rescue the kids," King says. The effects are likely to be more severe for children from lower-income families or whose mothers are not as supportive, she says.
But even good parenting might not stave off the metabolic downsides of maternal stress. The children of mothers who were under the most stress showed some worrying changes. By age 13, they were producing more insulin than normal, a possible prelude to diabetes, and about 14% of them were obese. The researchers found that the more stress a mother endured, the higher her child's body mass index (BMI). The BMIs of the children of high-stress mothers have continued to rise with age, and they may be susceptible to cardiovascular disease and other metabolic illnesses as they get older.
King says that studies that put animals under duress found the impacts on metabolism and behavior continued for at least four generations. Whether the children, grandchildren, and great-grandchildren of the Ice Storm group will share their problems remains to be seen.
Less Disastrous Disasters
The toll from disasters will probably climb. Social media now spread live videos of traumatic events to a large audience throughout the world, potentially distressing viewers who live far away, Morganstein notes. Moreover, wildfires, floods, and hurricanes are likely to become more frequent and destructive because of climate change.
A variety of measures can help reduce the health impact of natural disasters, however. Morganstein says that five interventions can protect against mental health disorders, including making the survivors feel safe, instilling hope, and providing a sense that their actions can make a difference. The last step is important because "a disaster can play on our sense of helplessness," he says. "We feel, 'What can I do against these forces?'" One way to counter that feeling, he notes, is for the government agencies and organizations responding to a disaster to make sure that survivors have a say in the recovery plan.
Research by Pruchno and others has identified people who could benefit most from interventions. She and colleagues found that the New Jersey residents most likely to develop PTSD after Hurricane Sandy shared several characteristics. Not only did they have weaker social connections, but before the storm they often were depressed, suffered from physical infirmities, earned less money, and had been unemployed for long periods. These people should be a focus for response plans and perhaps even candidates for evacuation, she says. "Most older people will do OK," she says. "We need to pay attention to people who are vulnerable when it looks like something bad is going to happen."
Scientists are also investigating new approaches to reduce the impact of disasters, including wildfires like the one that ravaged the Santa Cruz redwoods. Wearing masks and staying indoors can provide protection, but cutting inflammation might also spare the health of people who breathe smoky air. "There are a lot of drugs that middle-aged people like me live on that could be helpful," says Henderson, including aspirin. "We are at the point where we can think about clinical trials" or other types of studies to find out whether these drugs are beneficial.
By Mitchell Leslie
