The 10 patients who arrived at London’s Charing Cross Hospital in 1992 were desperate. No therapies had been able to tame the rheumatoid arthritis that was destroying their joints. As a last resort, they had agreed to participate in the first clinical trial to test a potentially risky treatment pioneered by immunologist Marc Feldmann and rheumatologist Ravinder Maini.
The two scientists had devised a novel strategy for soothing autoimmune diseases like rheumatoid arthritis, in which the immune system attacks patients’ own tissues. Their approach drew on Feldmann’s insights from almost a decade earlier about the roles of cytokines — the molecular messengers that orchestrate the immune system’s actions — in driving autoimmune diseases. The drug the patients received, the monoclonal antibody infliximab, stymied a powerful cytokine known as TNF α.

Feldmann and his scientific partner, Ravinder Maini, shared the 2003 Albert Lasker Clinical Medical Research Award for their work on TNF blockers.
The researchers weren’t sure what to expect from infliximab, but some of the patients, who had been admitted to the hospital because of worries about the drug’s safety, began to report improvements even before the first three-hour treatment was over. “They were telling us they felt really good, they no longer felt tired, and the world seemed clearer,” says Feldmann, who is now at the University of Oxford in the United Kingdom. And the patients continued to get better. One participant’s knee had been so badly inflamed it had ballooned to the size of a football. “The football was gone within two or three days,” says Feldmann, who shared the 2003 Albert Lasker Clinical Medical Research Award with Maini.
The success of infliximab in this study and follow-up clinical trials “transformed the pharmaceutical industry,” says immunologist and glycobiologist Raymond Dwek, also of the University of Oxford, who wasn’t connected to the TNF research. After Feldmann and Maini reported their early results with infliximab (Remicade), other companies got into the act with their own TNF inhibitors, spawning a family of new medications such as etanercept (Enbrel) and adalimumab (Humira). These drugs have become best sellers and proven beneficial for other illnesses driven by excess inflammation, such as Crohn’s disease, psoriasis, and ankylosing spondylitis. TNF inhibitors also inspired the development of drugs that target other cytokines.
Feldmann’s work on cytokines and autoimmune diseases set the stage for these advances. “He has had a tremendous impact,” says neuroimmunologist Lawrence Steinman of Stanford University. “Millions of people have had life-changing improvements in their illness because of his insights.”
Feldmann’s parents were Polish Jews who escaped the Holocaust thanks to his father’s gambit. Shortly before World War II, Feldmann’s father realized that a German invasion was inevitable and decided that the best way to survive was to join the Soviet army. As a volunteer he could choose his unit — he picked one that built airplane runways — and even wangled permission to bring along his wife. “They were behind the front — that was a good strategy,” says Feldmann, who was born in late 1944 while his parents were with the Soviet army, which was advancing on Berlin.
After the war, the family emigrated to France and then to Australia. When Feldmann arrived in Melbourne at age 8, he didn’t speak English and “expected to see kangaroos hopping down the streets.” Melbourne didn’t fit the storybook stereotype, but “it was a terrific place to grow up,” he says, because it welcomed immigrants and had a strong educational system.
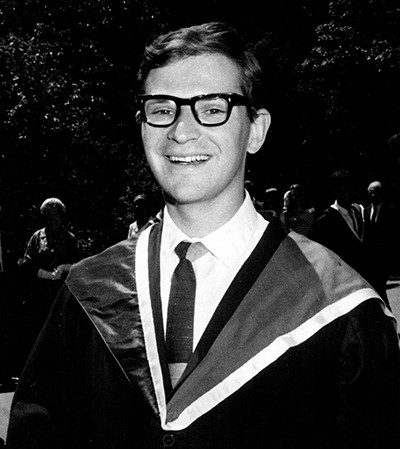
Feldmann graduated from the University of Melbourne in 1967. Shortly afterward he decided to begin immunology research.
Feldmann originally planned to become a doctor, not a scientist. He finished first in his class at the University of Melbourne but grew disenchanted with medicine after starting his hospital rotations. At the time, doctors often could do little for patients, he recalls. “Medicine as we understand it,” in which treatments have to pass muster in clinical trials, was in its infancy, he says.
A visit to Melbourne’s Walter and Eliza Hall Institute of Medical Research (WEHI), a hotbed of immunology research, suggested he would be happier in the lab. “I learned a huge amount at WEHI that made my career possible,” he says of his time as a PhD student at the Institute. One important lesson came from his dissertation project to devise better methods for nurturing immune cells outside the body. That know-how would prove crucial years later when he was investigating rheumatoid arthritis and TNF.
“But the most important thing I learned,” he says, “is the culture of collaboration. No single person can do anything substantial. You have to be part of a team.”
When Feldmann finished his PhD in 1972, Australian scientists who aspired to top positions were expected to gain experience in European or North American labs. Leaving the country was daunting because it would mean uprooting his wife and two small children. They decided to move to the United Kingdom for two years. The country turned out to be an excellent base for a scientist with his interests, he says, and they have only returned to Australia for visits.
Over his more than 50-year career, Feldmann established himself as one of the world’s premier immunologists. His achievements earned him ample recognition besides the Lasker Award, including the Crafoord and Tang prizes, the European Inventor of the Year, and membership in the Royal Society, the United Kingdom’s foremost scientific organization. His adopted home awarded him a knighthood, and his former home made him a Companion of the Order of Australia.
Dwek ascribes Feldmann’s success to several qualities. “I don’t know anyone with his breadth of knowledge,” Dwek says. Feldmann’s scientific vision was also critical, he adds. “Marc can take imaginative leaps. Unless you can do that, everything you do in life will be incremental.”
The intellectual leap Feldmann took in the early 1980s, when he was working at the Imperial Cancer Research Fund in London, opened the way for TNF blockers. He and his colleagues had been puzzling over the self-destructive attacks launched by the immune system in autoimmune diseases. Researchers had found that in parts of the body that are under attack in these illnesses, such as the joints or the thyroid, cells often produce large amounts of MHC class II proteins. These proteins are normally confined to certain types of immune cells, which use them to raise the alarm about invading pathogens. Why thyroid or joint cells would start churning out the proteins was a mystery.
Feldmann, who says he does his most creative thinking while out of the lab, had a revelation during a family vacation to Spain. He had been studying cytokines for more than a decade and realized that if they were out of whack, they could spur these cells to begin manufacturing MHC class II proteins. Instead of stimulating the immune system to combat pathogens, the misplaced proteins might then spark autoimmune attacks. The explanation sounds obvious now, he says, but at the time it was “heretical.” The idea was so outlandish, he recalls, that one pharmaceutical company refused to provide reagents for his team’s experiments to test it.

Feldmann hiking circa 1990
Undeterred, Feldmann and his colleagues began evaluating their heretical hypothesis by analyzing tissue samples from patients with autoimmune thyroid disease. However, they soon changed course because the therapies for this illness worked pretty well. As a result, Feldmann says, “there was no interest in funding new treatments or trials.”
Rheumatoid arthritis was a different story. The disease doesn’t just ravage the joints. It gnaws the heart, lungs, skin, and eyes, taking an average of seven years off patients’ lives. The therapies of the time could reduce pain and temporarily tamp down inflammation, but they couldn’t counteract the immune system malfunctions that drive the disease. Because patients needed better treatments, more funding was available for research.
Once Feldmann shifted his focus to rheumatoid arthritis, he applied the two lessons from his PhD days. First, he realized he needed to collaborate with an authority on the disease. At the suggestion of a former colleague, he contacted Maini, who walked into his office two days later. The pair hit it off and have been close friends ever since. They also complemented each other scientifically, and in 1985 Feldmann moved to the Charing Cross Sunley Research Centre, also in London, to make collaborating easier. The partnership with Maini was critical for the TNF research, Feldmann says. “I could never have done it without him.”
The second lesson from his PhD work enabled the scientists to extract vital data from samples of joint tissue surgically removed from patients with the disease. Feldmann says that at the time most researchers studying such samples were interested only in growing connective tissue cells in culture. They excluded the immune cells that are also abundant in the joint. But he and his colleagues wanted to know what the immune cells were up to. The culture techniques he developed as a graduate student allowed the team to cultivate mixtures of connective tissue and immune cells and to probe their interactions.
Experiments with these cell cultures implicated TNF as a wrongdoer in the disease. The molecule is just one of the inflammation-stoking cytokines prevalent in the joints of people with the disease, and at the time researchers weren’t sure how important it was. But when Feldmann and the team added antibodies that block TNF to their cell cultures, the levels of the other cytokines plunged, indicating that TNF was an inflammation manager.
This discovery put the bull’s eye on TNF in rheumatoid arthritis. But Feldmann and his colleagues didn’t have to create TNF-blocking drugs from scratch. Pharmaceutical companies were already making them as potential treatments for sepsis, a body-wide inflammation often spurred by infections. Feldmann recalls that when he and his colleagues approached several of these companies about launching clinical trials of the antibodies in rheumatoid arthritis, all but one refused. They didn’t think tackling one cytokine would curtail inflammation, which results from the actions of many molecules, and worried about possible side effects such as infections. The one company that agreed, Pennsylvania-based Centocor, manufactured what became known as infliximab.
Feldmann and Maini launched a new collaboration with the company that led to clinical trials of infliximab in patients with rheumatoid arthritis and its eventual approval in the late 1990s. Other companies also developed TNF-targeting antibodies, and these treatments became the top-selling drugs in the world for more than 10 years, knocked from the top spot only in 2021 by COVID-19 vaccines, says Feldmann. “That’s a pretty good record.”
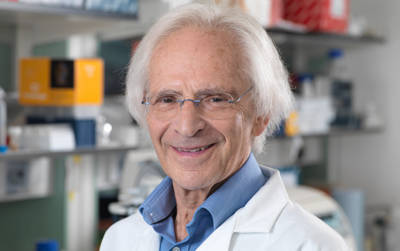
Feldmann continues to investigate new approaches for treating conditions such as Alzheimer’s disease.
Feldmann’s influence on science extends well beyond his work on TNF, says Dwek. For more than a decade he headed the Kennedy Institute of Rheumatology, a top center for immunology research, and shepherded its merger with the University of Oxford. Feldmann has also made it his mission to foster research that leads to new therapies. Starting in 1984 and continuing until COVID-19 intervened, he and his colleagues convened an annual conference at Oxford where scientists and clinicians could discuss new ideas and mingle with industry representatives who might fund them.
“My career success is translating molecular insights into therapies,” Feldmann says. He continues to pursue that goal and has co-founded several biotech firms that are developing treatments for conditions such as Alzheimer’s disease, Parkinson’s disease, and heart attacks. He hopes that through the teamwork he has always extolled, these new companies will deliver breakthroughs on par with TNF inhibitors.
By Mitchell Leslie

