 Nancy Wexler is Higgins Professor of Neuropsychology in the Departments of Neurology and Psychiatry of the College of Physicians and Surgeons at Columbia University. She is also the president of the Hereditary Disease Foundation. She is most widely known for her important scientific contribution to understanding Huntington’s disease. Since 1979, Wexler has led a research study in Venezuela of the world’s largest family with Huntington’s disease, developing a pedigree of over 18,000 individuals and collecting over 4,000 blood samples, which helped lead to the identification of the Huntington’s disease gene at the tip of human chromosome 4. One result of this work was the development of a presymptomatic test that could identify those who carry the fatal gene prior to the onset of symptoms. For her contribution to research, policy, and advocacy for Huntington’s disease, Wexler received the Albert Lasker Public Service Award in 1993.
Nancy Wexler is Higgins Professor of Neuropsychology in the Departments of Neurology and Psychiatry of the College of Physicians and Surgeons at Columbia University. She is also the president of the Hereditary Disease Foundation. She is most widely known for her important scientific contribution to understanding Huntington’s disease. Since 1979, Wexler has led a research study in Venezuela of the world’s largest family with Huntington’s disease, developing a pedigree of over 18,000 individuals and collecting over 4,000 blood samples, which helped lead to the identification of the Huntington’s disease gene at the tip of human chromosome 4. One result of this work was the development of a presymptomatic test that could identify those who carry the fatal gene prior to the onset of symptoms. For her contribution to research, policy, and advocacy for Huntington’s disease, Wexler received the Albert Lasker Public Service Award in 1993.
Q: What motivated the establishment of the Hereditary Disease Foundation?
A: In 1968, we were living in Los Angeles. My mom was crossing the street early one morning going to jury duty, and a policeman just screamed at her: “How can you be drunk so early in the morning? Shame on you!” Of course, she wasn’t drunk. She saw a neurologist that day and was diagnosed with Huntington’s. My father established the Hereditary Disease Foundation that year. We discovered that her own father had died of Huntington’s, and all three of my mother’s brothers were diagnosed with different stages of Huntington’s in 1955. Gradually, my mother lost the ability to feed herself, walk, talk. She also tried to commit suicide. Fortunately, she didn’t go crazy — a lot of patients that I know have hallucinations. Huntington’s affects all parts of your body — your movement, your mind, your thinking, and your mood. It is a ghastly death over 10–20 years. Once you inherit the abnormal gene, it eventually shows up and kills you — 100%.
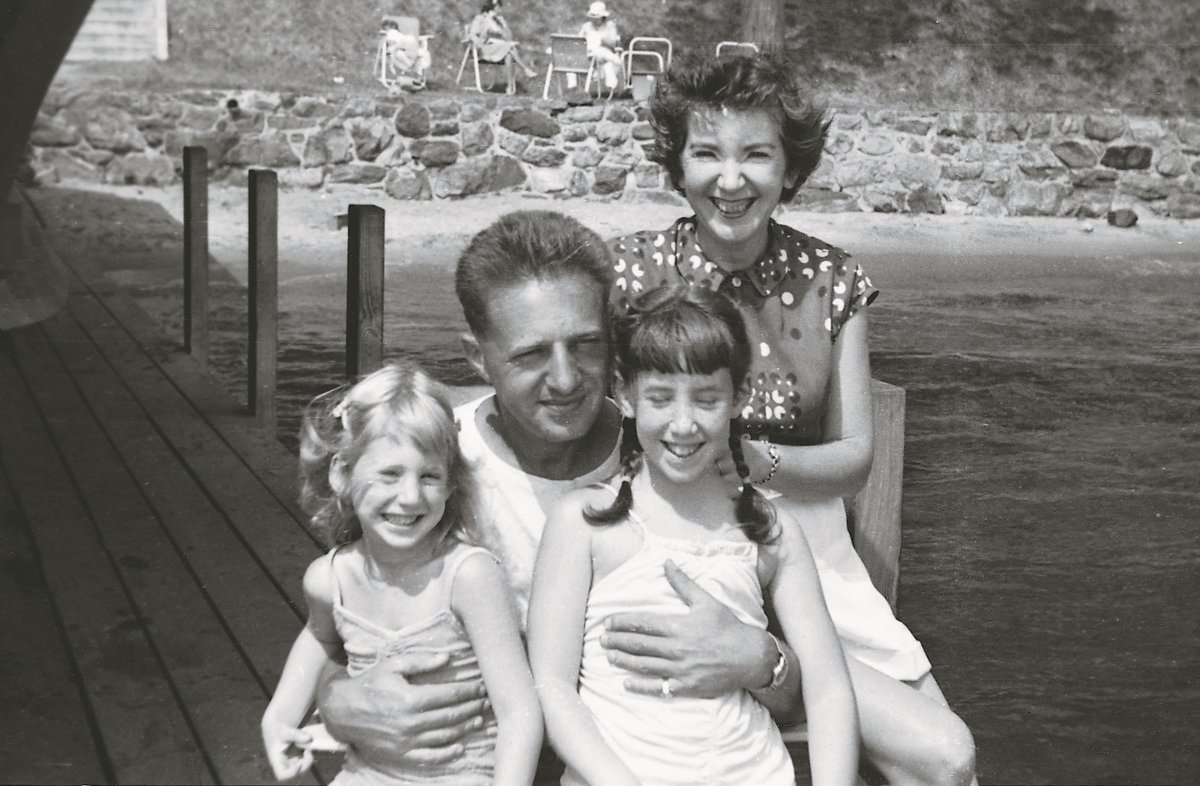
Milton Wexler and Leonore Wexler with their daughters Alice and Nancy (right).
Q: Was there funding for research in Huntington’s at that time?
A: No money and no science. George Huntington, who got his medical degree here, at Columbia, had written an article in 1872 describing Huntington’s and its hereditary pattern. And he mentioned that both men and women get it equally. Huntington was ahead of his time. He really described a dominant pattern before we even knew what dominance was. But there was nobody really doing any research on it.
Q: How did you go about motivating research in Huntington’s disease? What were the first steps?
A: At the time when my mom got diagnosed, my dad was running therapy workshops for creative people. My dad was a clinical psychologist; he was really a genius, extremely creative, very innovative, and very supportive. Since he was doing that with artists, and architects, and writers, he said let’s do it also with scientists. We didn’t show slides or give speeches but asked participants to just focus on the conversation. In 1968, we had the very first workshop in California. The geneticist Seymour Benzer, who was at Caltech, helped establish a fabulous science advisory board. Right from the beginning, he said we need to fund the most innovative and creative scientists. We didn’t give very big grants — $5,000 or $10,000 back then. Today we have grants that are $25,000 or $50,000 per year.
Q: It is often said that foundations and philanthropy in general tend to fund riskier projects — new and creative ideas that would have a hard time getting funded otherwise.
A: My dad would always encourage my sister and me; he would say, “Don’t let life defeat you before you get started.” Yes, it might fail. Yes, it might not work. But if you defeat yourself before you try, that is terrible. Because then you’ve lost, and, potentially, the world has lost.

Lake Maracaibo communities
In the ‘70s, Brown and Goldstein [Michael Brown and Joe Goldstein, who later won both a Lasker Award in Basic Medical Research and a Nobel Prize in Physiology or Medicine] had just been able to figure out the biochemistry of a cholesterol disease called familial hypercholesterolemia by studying a family with two heterozygote [one faulty gene copy] parents and their daughter who was a homozygote [two faulty gene copies]. So we thought we needed homozygotes. But Huntington’s is shockingly rare. In July 1979, I went to Venezuela because I had heard about a community on Lake Maracaibo where people with Huntington’s were intermarrying because they were stigmatized and ostracized by the rest of the community. In a stilt village on the lake, we found a man sitting in a hammock who clearly had Huntington’s, and his wife had Huntington’s. They had 14 living children, and out of the 14 kids, 10 got Huntington’s. And some of them were homozygotes, but that didn’t make them sicker, which was shocking to us because we thought having twice of the faulty gene would make you twice as sick.
Around that time, scientists were talking about the potential existence of small irregularities in the DNA. PCR didn’t exist yet. People were doing just a tiny bit of sequencing and trying to look at our DNA using something called restriction fragment length polymorphism [RFLP]. That was the state of the art then. We gave David Housman $6,000 in 1970 to look for these markers and see if they segregated with the disease.
In October of 1979, we had a workshop at the NIH [US National Institutes of Health], and we looked for a way that we could actually use these little RFLPs to find the Huntington’s gene. Every time you would find a new marker, you needed to see if that marker would actually travel [segregate with the sick individuals] in a family with Huntington’s. There was huge commotion at the workshop; people argued and argued — how many years would it take? 50? 100? Was it even possible? Some of the scientists said that if we were telling people that we are looking for a Huntington’s gene, we were misleading the families — it was unethical because it was not going to happen. Ray White and David Botstein, who were friends, said, “Nancy, I don’t think we should do that.” We knew that we had to have a really big family in order to see if the marker would travel with the disease, and I had just come back from visiting a gigantic family in Venezuela, so we started looking for markers and combined that work with studying homozygotes.
Q: Was it difficult to persuade the local families to participate? From their perspective, you were outsiders coming to their small fishing villages asking them for samples. They probably didn’t understand genetics and the details of your science.
 A: They were suspicious of us. The families were living in total poverty. I explained that Huntington’s is also in my family, and in the United States, and in the world. At first they didn’t believe me. How could that be? They said something so poignant, so touching: “You got to the moon and back, why can’t you cure Huntington’s?” Which was so true! We decided to create a nursing home for them right on the edge of Maracaibo. That entire area was a slum. It had the worst bar in town, called the Red Bull Bar: prostitutes, drugs, heroin. We actually got the government to tear down the Red Bull Bar. But then it took 10 years for the government and philanthropy to help us create the clinic, which was open in the 1980s. We were taking care of 66 people — we fed them pureed food, because people with Huntington’s need like 5,000 calories a day. We loved them, they were part of our own family. The clinic is still open today. We’ve given $17 million ever since the clinic opened.
A: They were suspicious of us. The families were living in total poverty. I explained that Huntington’s is also in my family, and in the United States, and in the world. At first they didn’t believe me. How could that be? They said something so poignant, so touching: “You got to the moon and back, why can’t you cure Huntington’s?” Which was so true! We decided to create a nursing home for them right on the edge of Maracaibo. That entire area was a slum. It had the worst bar in town, called the Red Bull Bar: prostitutes, drugs, heroin. We actually got the government to tear down the Red Bull Bar. But then it took 10 years for the government and philanthropy to help us create the clinic, which was open in the 1980s. We were taking care of 66 people — we fed them pureed food, because people with Huntington’s need like 5,000 calories a day. We loved them, they were part of our own family. The clinic is still open today. We’ve given $17 million ever since the clinic opened.
Q: You started the research in 1979, and by 1983 the chromosome on which the gene resides was identified. So it took a lot less than 50 or 100 years.
A: But can I tell you why? There is a part of the Huntington’s gene where the DNA is repeated over and over and over again. It spells a word called CAG, for glutamine. You need to have glutamine, but our gene just gets overly enthusiastic. It’s like an odd switch, turned [on] over and over again, so the poor gene just keeps making CAG, CAG, CAG. A normal human will have 17–24 CAGs. There was a little boy — he had nine siblings, and seven out of nine had Huntington’s — he had 120 repeats. His gene was so gigantic that you could actually identify it just by looking at its DNA sequence.
The gene hunters were total heroes: Michael Conneally, David Housman, Francis Collins, John Wasmuth, my other half [Herb Pardes], Bob Horvitz, and Gill Bates. [They were able to] figure out that the gene was on top of chromosome 4.
Tom Maniatis was developing markers, and he had developed a 12th one. At first, we tried it looking at a family in Iowa that we thought would be big enough to show if it was the right marker in the right place. It wasn’t. We were almost going to give up. But we had all this DNA from the Venezuelans, so we popped that right in, and, lo and behold, the 12th marker showed up on the top of chromosome 4. It was screamingly significant. There was no possibility that it was by chance. We said, “Wow, this is actually where the Huntington’s gene is!” But finding the gene itself — that took a lot longer.

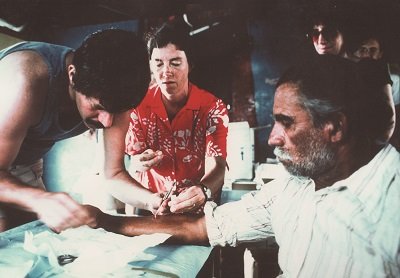
The Huntington’s Disease Collaborative Research Group “The Gene Hunters” during a working vacation at Dennis Shea’s retreat in the Florida Keys.
Q: How did you find the gene?
A: Since it took 3 years to find the marker, everybody thought finding the gene would be a piece of cake. But the gene hunters took 10 years to go from the marker to finding the gene itself. That was surprising. We said to all the scientists, “We are going to support you, but we want you to agree to collaborate, and you have to publish finding the gene as a collaboration.” And they agreed. It just changed the attitude, because people would walk in and they would say, “Here is something that I just found, I don’t know where it is on the chromosome, can you check it, can you test it?” Every single person completed [a piece of] that story. The gene hunters invented 14 different technologies while looking for the gene. Those technologies helped other gene searchers for Alzheimer’s, dwarfism, and Lou Gherig’s.
Q: This was in 1993; did you expect that it would take this long to develop a cure for Huntington’s?
A: No. That has been the disappointing part. We have had lots of workshops to discuss strategies that could affect Huntington’s and we have supported many scientists, including Beverly Davidson at The Children’s Hospital of Philadelphia, to pursue these promising strategies. The very first huntingtin-lowering therapy is being tried in people right now. I just met a patient who has enrolled in the trial in London — he had a little Band-Aid on his back, he had just gotten a gene therapy shot. It was very moving. He said that his mom died of Huntington’s with no hope, and I congratulated him on being a pioneer — the first person in the world to try this therapy.
Q: What is next?
A: We have been looking for genetic modifiers. We have 23 years’ worth of clinical data. We have neurological exams on 20,000 people. By studying the Venezuelan families, we’ve identified that people get Huntington’s from age 2 to 92. There is a lot of variability among persons with Huntington’s, which led us to think that maybe there are other genes that can really influence when you get sick.
Q: What did getting a Lasker Award mean to you?
A: It is hard to put into words; it was so meaningful! And it was very magical. At that time, my dad was still alive and healthy. And Mary Lasker was alive. I thought, I’ve clearly died and gone to heaven. Hillary Clinton was the speaker — she was the First Lady at the time — and she gave a fabulous speech. Getting a Lasker Award was so edifying and gratifying. It was also confirming, because here I was doing sort of outlandish things — all of this research we were doing was very cutting edge. There are scientists, myself included, that are insecure. How could your science be good if you’re not insecure? The Lasker Awards changed how people treated me. It was such a validation of what I was trying to do. The way that the Lasker Awards are given is very careful and thoughtful, and the Lasker Foundation recognizes people early on. Nobody was recognizing us in ’93; we had just found the gene and published it, for God’s sake. The Lasker Foundation really legitimized what we were doing, what I was doing even, as a young woman. Mary Lasker had a unique vision.

Left to right: Michael DeBakey, Günter Blobel, Nancy Wexler, Paul Rogers, Donald Metcalf
Q: What could you do with more money?
A: It took 3 years to find a marker and 10 years to find the gene, and now how long will it take to find a cure? The science gets better. We have 400 people being sequenced, but we don’t have the money, so their data are all just sitting there. We are always fundraising like maniacs. So technology helps, but it still needs to get faster and cheaper. We are hopeful that whatever we find by sequencing will help not only Huntington’s but other brain bandits. The NIH budget is getting cut, so philanthropy is trying to do more. The Neurology Institute at the NIH [NINDS, National Institute of Neurological Disorders and Stroke] just had a stroke of genius. They have tenure awards where if we had consistent funding from them for a couple of years, we could apply for something that lasts for 10 years because they know if you are going to make a difference in brain disease, it takes time. It takes time to build a team and to get them to collaborate. It doesn’t have to be just publish or perish — it’s a horrible pressure on scientists. So I think the Neurology Institute, under Walter Koroshetz, is really trying to be innovative.
