Szent-Gyorgyi soon discovered that he could isolate hexuronic acid from oranges, lemons, and cabbages, all of which were believed by nutritionists to be rich in vitamin C, a postulated substance that had never been isolated. Recall that a deficiency of vitamin C causes a debilitating disease called scurvy that occurred in sailors who were deprived of fresh fruits and vegetables for long periods of time. In 1932, when Szent-Gyorgyi made the connection in his mind that hexuronic acid might be vitamin C, he had just enough crystalline hexuronic acid to do one experiment. He injected his precious little hexuronic acid into several guinea pigs with scurvy. Eureka! Hexuronic acid cured scurvy in the guinea pigs, suggesting that hexuronic acid and vitamin C might be one and the same. This was a terrific experiment that solved a longstanding problem in medical science. However, Szent-Gyorgyi soon found himself in an embarrassing situation. He had no more purified hexuronic acid to repeat the experiment. The best source of hexuronic acid was the adrenal gland from cows, but they were no longer available to him. Although orange juice and lemon juice had high levels of hexuronic acid, they contained many other related sugars that made purification extremely difficult. Szent-Gyorgyi solved the problem through an intuitive leap of the imagination.
Szent-Gyorgyi was working in Szegred, Hungary, the paprika capital of the world. Paprika is a dried ground pepper. In Hungary, it is not only a spice but a national tradition. Matching salt and paprika shakers are found on every restaurant table. Unlike most Hungarians, Szent-Gyorgyi was not fond of paprika. One night his wife served him fresh red paprika for supper. As he wrote in his autobiography, “I did not feel like eating it so I thought of a way out. Suddenly it occurred to me that this is the one plant I had never tested. I took it to the laboratory and about midnight I knew that it was a treasure chest full of vitamin C. Two milligrams per gram.”
Within several weeks Szent-Gyorgyi had produced three pounds of pure crystalline hexuronic acid—enough to clearly show in his vitamin C-deficient guinea pigs that hexuronic acid was equivalent to vitamin C. This is a beautiful example of Szent-Gyorgyi’s dictum—seeing what everyone has seen, but thinking what no one has thought.
In 1937, only several years after the discovery of vitamin C, Szent-Gyorgyi received the Nobel Prize, which Timemagazine dubbed the Paprika Prize. That year, the deliberations in the Nobel Committee apparently centered on whether the Prize should go to Szent-Gyorgyi alone or be shared with several other scientists doing similar work based on Szent-Gyorgyi’s original insight. In the end, the Prize was given to Szent-Gyorgyi alone, but the deliberations were apparently so long and acrimonious that when the chairman of the Nobel Committee in Medicine or Physiology, Hans Christian Jacobaus, came out to make the announcement, he dropped dead of a heart attack right on the spot!
Like Nobel Jury deliberations, Lasker Jury deliberations are always lively and on occasion there have been heated discussions about whether the award should go to one area of science or another and who should receive it. But this year our Lasker Jury had an easy job and reached a unanimous decision to award the Basic Medical Research Award to Robert Furchgott and Ferid Murad for their ingenious discoveries that paved the way to understanding the role of nitric oxide in health and disease. Nitric oxide is an unstable gas that has powerful biologic effects in all animals from fruit flies to humans. The effects of nitric oxide in the body are just as powerful and just as widespread as those of conventional hormones that were discovered much earlier, such as the steroid hormones (glucocorticoids, estrogen, and testosterone), the prostaglandins, and the cytokines. The story behind the discovery of nitric oxide is just as fascinating as the story of vitamin C. It illustrates the essence of all basic discoveries—a constant dialogue between imagination and experimentation.
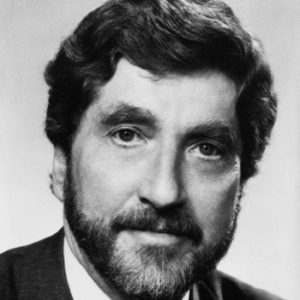
In 1975, Ferid Murad, a biochemist, discovered that chemicals such as nitric oxide and nitroglycerin stimulate the enzyme that produces cyclic GMP, the intracellular signaling molecule that causes smooth muscle cells to relax. Murad believed that this action explained the blood vessel-dilating activity of nitroglycerin, and he coined the term nitrovasodilators to denote this class of agents. His suggestion that the body might produce nitric oxide as a signaling molecule seemed outrageous at the time, since nitric oxide is an unstable gas.
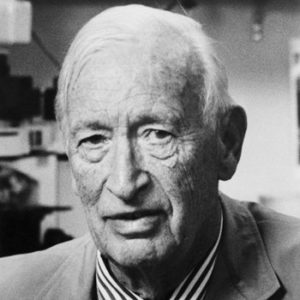
In 1980, Robert Furchgott, a physiologist, carried out a brilliantly designed experiment in which he rubbed off the innermost layer of a blood vessel and discovered a labile agent that caused the vessel’s smooth muscle cells to relax. Surprisingly, this agent was produced by the rubbed off endothelial cells that line the blood vessels, yet it acted on the underlying smooth muscle. Furchgott named this labile molecule endothelium-derived relaxing factor (EDRF).
At first the work of Murad and Furchgott seemed totally unrelated, but then in the mid-1980s it converged in a dramatic way when the two scientists found that EDRF relaxed smooth muscle by activating the enzyme that produces cyclic GMP, in virtually the same way that nitrovasodilators work. This led to the prediction that EDRF is nitric oxide, analogous to Szent-Gyorgyi’s prediction that hexuronic acid is vitamin C. By 1987, several groups of scientists, including Salvador Moncada and Louis Ignarro, confirmed that EDRF and nitric oxide are one and the same. This triggered an explosion in the nitric oxide field, opening the floodgates of discovery. During the last 12 months, 4,500 papers on nitric oxide were published in the scientific literature—500 more than on cholesterol, and 4,000 more than on vitamin C! This nitric oxide explosion could not have occurred without the prior decade of groundbreaking work initiated by Furchgott and Murad.
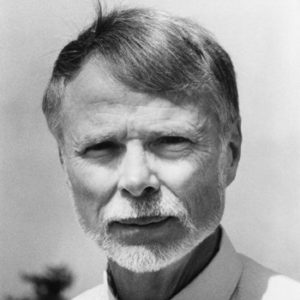
 The story of Szent-Gyorgyi’s discovery of vitamin C is a beautiful illustration, and it is directly comparable to the discovery of nitric oxide, which we honor today with the Albert Lasker Basic Medical Research Award. Szent-Gyorgyi began his scientific career by studying the chemical changes that occur when foodstuffs—carbohydrates, fats, and protein—undergo combustion when they are burned by cells—a process called biological oxidation. In the course of his studies he isolated a molecule from adrenal glands that lost and regained hydrogen atoms—a hydrogen carrier. This molecule contained six carbon atoms, had the properties of a sugar and an acid, and was originally named hexuronic acid (later renamed ascorbic acid).
The story of Szent-Gyorgyi’s discovery of vitamin C is a beautiful illustration, and it is directly comparable to the discovery of nitric oxide, which we honor today with the Albert Lasker Basic Medical Research Award. Szent-Gyorgyi began his scientific career by studying the chemical changes that occur when foodstuffs—carbohydrates, fats, and protein—undergo combustion when they are burned by cells—a process called biological oxidation. In the course of his studies he isolated a molecule from adrenal glands that lost and regained hydrogen atoms—a hydrogen carrier. This molecule contained six carbon atoms, had the properties of a sugar and an acid, and was originally named hexuronic acid (later renamed ascorbic acid).