One day in 1993, a small, nondescript package arrived at Brian Druker’s new lab at the Oregon Health & Science University (OHSU). Tucked into the box were five vials about two inches long, each containing a smidgen of white crystals. Biochemist Nicholas Lydon and colleagues at the pharmaceutical company Ciba-Geigy in Switzerland had synthesized the compounds in the vials, and Druker’s challenge was to gauge whether any of them killed cancer cells from patients with chronic myeloid leukemia (CML), then a lethal disease.
Although Druker was still unpacking his equipment, he got to work. One compound with the prosaic designation CGP 57148 clobbered leukemia cells, he found. “It was dramatic how big an effect there was over a thousand-fold concentration range,” says Druker, who now directs the Knight Cancer Institute at OHSU.
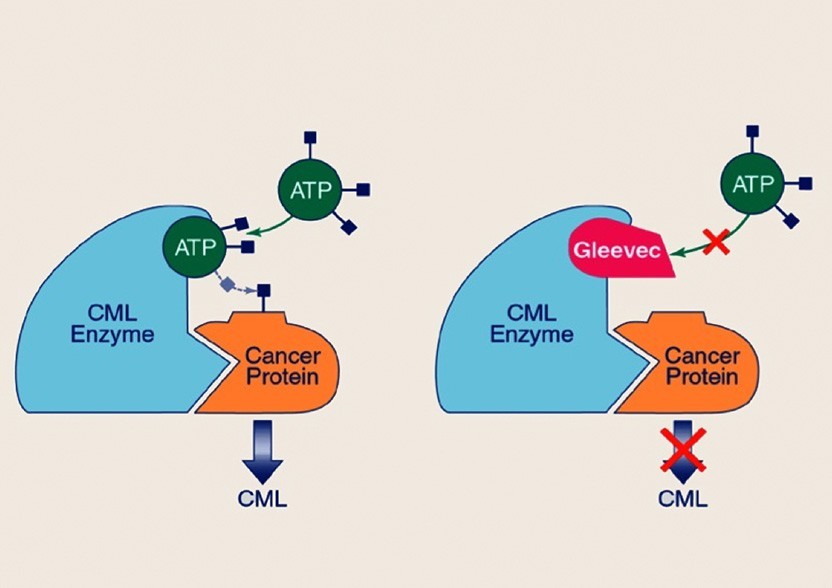
Schematic model for the mechanism of action of Gleevec
Image courtesy of OHSU/Kristyna Wentz-Graff
After further testing and tinkering, CGP 57148 would become imatinib (Gleevec), a drug that, when it was approved by the US Food and Drug Administration in 2001, Time magazine described as “a breakthrough — not only for what it does, but more importantly, for the revolutionary strategy it represents.” For discovering the drug and shepherding it through clinical trials, Druker and Lydon shared a 2009 Lasker Award with Charles Sawyers, Memorial Sloan Kettering Cancer Center.
Imatinib proved revolutionary for patients with CML because it stretched their life expectancy from 3 or 4 years after diagnosis to decades, if they started treatment early. But the drug also broke new ground intellectually as the first ‘smart’ cancer therapy.

Left to right: Charles Sawyers, Brian Druker, and Nicholas Lydon
Imatinib slayed cancer cells by exploiting their genetic faults, and unlike radiation and chemotherapy, it spared healthy cells. The drug demonstrated that researchers can develop treatments that attack specific varieties of cancer “if we target the key molecular drivers of cancer cell growth and survival,” says Druker. “That’s a remarkable change.”
Since the first Lasker Awards were presented in 1946, knowledge about cancer has undergone a remarkable change, and winners of the award have revolutionized how scientists think about the disease. Lasker Award recipients have uncovered the genetic seeds of tumors within our own cells, connected broken chromosomes to cancer pathogenesis, and shown how to enlist the immune system to battle the disease — and possibly even to eliminate some types of cancer. Their work and research by other scientists is now paying off with more powerful and less harmful treatments, as well as preventive cancer vaccines. In addition, Lasker winners helped transform the public’s view of cancer, rescuing the disease from polite euphemisms or silence and transforming it into one for which the public actively campaigns for understanding and research support.
When the awards started, the outlook for people who developed cancer was grim. At the time, only about 35% of patients lived for 5 years after their diagnosis. By comparison, 67% of patients now survive that long, according to recent data from the National Cancer Institute. Researchers have long known what goes wrong in the disease. Cells start dividing out of control, proliferating, and spreading until they often kill the patient. But why cells start behaving so selfishly remained murky. Was it viruses? Exposure to environmental insults such as toxic chemicals? Or maybe genetic errors? Even cloudier was researchers’ conception of how any of these possible triggers could upset the finely tuned process of cell division and unleash rampant growth.
Even in the early 1970s, says J. Michael Bishop of the University of California, San Francisco (UCSF), scientists were still at a loss to explain how cancer arises. “There were hints, but nobody had put it together,” he says. “There was no credible theory of cancer.”
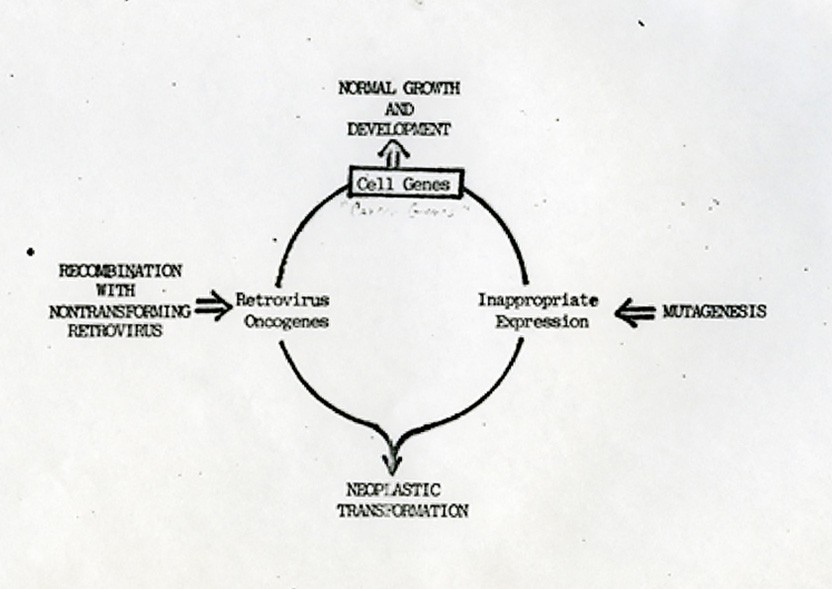
A cartoon schematic drawn in 1982 by Varmus and Bishop detailing how normal genes (proto-oncogenes) that control growth and development can become cancerous (neoplastic).
Image courtesy of the UCSF Archives & Special Collections
But he and his colleagues were about to add a key insight that would lead to one, thanks to a virus that infects chickens. When Bishop started at UCSF in 1968, he planned to probe the replication of the poliovirus. Then a colleague showed him what happens when the Rous sarcoma virus — named for the 1958 Lasker winner and 1966 Nobel laureate Peyton Rous of Rockefeller University — invades fibroblasts from a chicken embryo. It transforms the cells, that is, it makes them cancerous. Through the microscope, Bishop saw that fibroblasts, normally sprawling and angular, rounded into balls after infection. And instead of respecting each other’s personal space, they started to pile atop one another. “They have no social contract whatsoever,” says Bishop.
He was enthralled. “The virus had the genetic equipment to transform a cell overnight,” Bishop says. He wanted to know how it could engineer such a dramatic change, and he worked with his new colleague Harold Varmus — who went on to head the National Cancer Institute, the National Institutes of Health, and the Memorial Sloan Kettering Cancer Center and now works at Weill Cornell — to find out. A mutant Rous sarcoma virus that lacked a chunk of its genome provided a clue. Although the mutant still infected cells and reproduced, it didn’t make them cancerous, indicating that the cancer-inducing gene, known as src, must reside in the missing section of the genome.
The transforming gene might be part of the virus, Bishop and Varmus reasoned, or the virus might have swiped it from a host. The researchers concocted a DNA probe to determine whether src had a twin in other organisms. Bishop, Varmus, and colleagues tested a variety of bird species, measuring how tightly the probe attached to their DNA, and discovered that this genetic double was ubiquitous, a result they published in 1976. “We found it in chicken DNA, and the next year we showed that it was in every bird we tested, down to the emu,” the flightless Australian bird that is a distant relative of the other species, says Bishop.
At first, the scientists couldn’t detect a comparable gene in mammals, but it then showed up after they tweaked their experimental conditions. “When we found it in bird DNA, people were electrified,” Bishop says. “When we found it in human DNA, that ignited a firestorm.” The discovery meant that “there is a precursor of a cancer gene in normal cells,” he says.
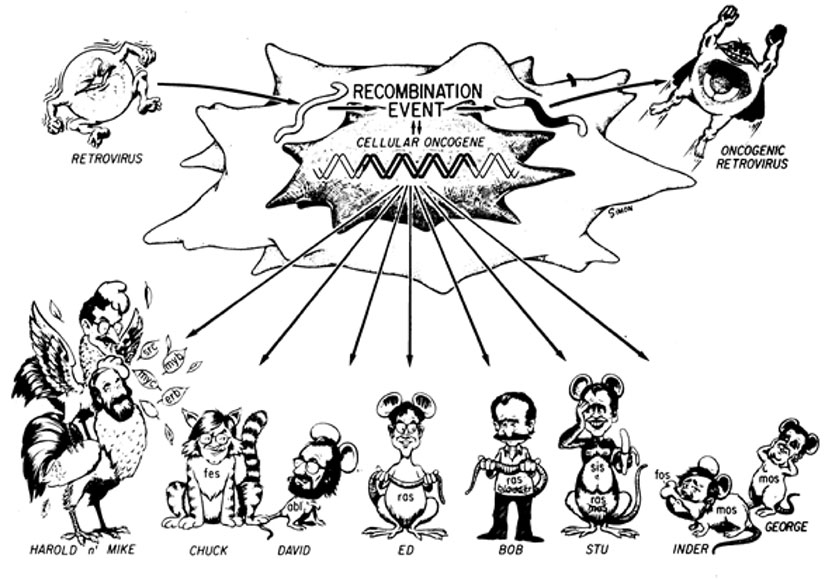
A cartoon drawn by Jamie Simon of the Salk Institute for the cover of the 1983 Cold Spring Harbor RNA Tumor Virus Meeting program. The upper half of the cartoon depicts a virus hijacking a normal cellular gene, converting the gene into a viral cancer-causing oncogene, and producing the supervillain virus on the right. Varmus’ and Bishop’s use of these villainous viruses in chickens to discover the underlying normal gene inspired many other scientists to do the same, using other cancer-causing viruses in other model organisms. The lower part of the cartoon depicts a number of other famous scientists as the animal species they chose to work with and the proto-oncogene they discovered. Image courtesy of Jamie Simon, Salk Institute
These cancer gene precursors, scientists now know, are proto-oncogenes. More than 40 of them have come to light, and they perform vital duties in cells. The human version of src, for instance, spawns a protein that relays messages that stimulate cells to grow, move, or specialize. Mutations corrupt these beneficial genes, turning them into oncogenes that promote cancer growth. Oncogenes can’t instigate cancer alone, however. Mutations also have to disable tumor suppressor genes that normally rein in cell division — an idea first proposed by another Lasker recipient, Alfred Knudson of the Fox Chase Cancer Center. The discovery by Bishop, Varmus, and their colleagues “set up research for the next 40 years,” says Charles Sherr of St. Jude Children’s Research, who served on the Lasker Research Awards Jury between 1998 and 2006.

Harold Varmus (left) and Michael Bishop in 1989
In 1982 Bishop and Varmus shared a Lasker Award with three other researchers, including Hidesaburo Hanafusa, then at Rockefeller University, who worked out how the Rous sarcoma virus picks up src; Raymond Erikson, who identified the first protein encoded by a form of src in chickens when he was at the University of Colorado; and Robert Gallo for his work at the NIH on the human T cell leukemia virus. Bishop and Varmus received a Nobel Prize in 1989.
Two more Lasker Award winners rewrote scientific consensus by showing that broken or rearranged chromosomes, which often litter cancerous cells, could be a cause of the disease, not just a consequence.

Janet Rowley
Image courtesy of Chicago Tribune
In 1972, Janet Rowley of the University of Chicago discovered that in patients with CML, portions of chromosomes 9 and 22 had swapped places, resulting in a shrunken chromosome 22.
In the late 1950s, Peter Nowell of the University of Pennsylvania and David Hungerford of the Institute for Cancer Research had first noticed this puny chromosome, later named the Philadelphia chromosome, but they couldn’t determine its identity. Nowell and Rowley shared a Lasker Award in 1998 with Knudson; Hungerford died before the Award was given for his work.

Peter Nowell (left) and David Hungerford
These insights sparked imatinib’s discovery because, as other researchers revealed, the chromosome exchange fuels CML. A section of the BCR gene from chromosome 22 merges with a portion of the ABL1 gene from chromosome 9. The hybrid protein resulting from this union, BCR-ABL1, is manic, constantly prodding cells to divide.
That’s where Druker came in. Hoping to find a drug that would thwart BCR-ABL1, he contacted researchers at pharmaceutical companies to find out if they had any candidates. By coincidence, the first person he called, his friend Nicholas Lydon, was working on the same problem and had compounds ready to test. The pair later joined with Sawyers, who had been studying BCR-ABL1 for almost a decade, and other scientists to run a clinical trial of the drug. CML causes a surge in white blood cells in the circulation. As the researchers revealed in 2001, imatinib knocked the cell numbers down to normal in 98% of patients who received the highest doses — results that led to the drug’s approval later that year.
Sawyers and his colleagues went on to crack the mystery of why some patients become resistant to imatinib, discovering that these people carried mutations that warped BCR-ABL1 so that imatinib could no longer block it. That finding spawned a new drug, dasatinib (Sprycel), that attaches to BCR-ABL1 in a slightly different way and jams mutated versions of the protein.

From left to right: Dennis Slamon, Axel Ullrich, Michael Shepard at the 2019 Lasker Awards ceremony
The success of imatinib and another drug approved three years before, trastuzumab (Herceptin), opened the floodgates for therapies that attack specific vulnerabilities of cancer cells. Trastuzumab, which transformed breast cancer treatment and has been prescribed for more than 2.3 million patients, was the brainchild of the researchers who received a 2019 Lasker Award. They are Dennis Slamon of the University of California, Los Angeles; Axel Ullrich, now at the Max Planck Institute of Biochemistry in Germany; and H. Michael Shepard, who was then at Genentech. The rationale for the drug is that around 20% of breast tumors — as well as several other cancer types — make excess amounts of a protein called HER2 that fosters their growth. Trastuzumab is an antibody that latches onto HER2 and inhibits tumor growth.
Lasker winners pioneered other lifesaving approaches that use the immune system to fight tumors or the viruses that cause them. The immune system is capable of destroying tumors, but unfortunately, it often leaves them alone. James Allison, now at the University of Texas MD Anderson Cancer Center, and his colleagues uncovered one reason why. T cells, key fighters in the body’s anti-tumor forces, sport an inhibitory protein called CTLA-4 that prevents them from going on the attack. Allison suspected that CTLA-4 was switched on in some cancers and stopped T cells from combating the tumors. He and his colleagues tested the idea by injecting an antibody that throttles the protein into mice with tumors. The antibody treatment resulted in slowed growth of the tumors, the scientists reported in 1996.

Jim Allison
Image courtesy of University of Texas MD Anderson Cancer Center
That CTLA-4–blocking antibody gave rise to ipilimumab (Yervoy), which in 2010 became the first drug to boost survival of patients with previously unresponsive melanoma in a phase III trial. Even more impressive, ipilimumab, which the Food and Drug Administration approved in 2011, seems to have cured some of these patients, who were alive more than a decade after the treatment. Ipilimumab was the first in a new class of drugs, called checkpoint inhibitors, that have dramatically improved the prospects for patients with several types of cancers, including melanoma, renal cell carcinoma, and non-small cell lung cancer. An additional six checkpoint inhibitors have joined it in the pharmacopoeia. For his work on CTLA-4, Allison earned a Lasker Award in 2015 and shared a Nobel Prize in 2018 with Tasuku Honjo of Kyoto University in Japan, who discovered a T-cell off-switch called PD-1 that other checkpoint inhibitors target.

Douglas Lowy (left) and John Schiller
2017 Lasker Award recipients John Schiller and Douglas Lowy of the National Cancer Institute recruited the immune system to fight tumors in a different way, helping to devise a vaccine against human papillomavirus (HPV). Infections by some types of the virus, most often the variety HPV16, induce cervical cancer, the third leading cause of cancer deaths in women, with more than 250,000 victims worldwide each year. “You don’t need to be Einstein to see that if you prevent the viral infections, you prevent the cancers,” says Schiller.
The researchers first took aim at the similar bovine papillomavirus (BPV). To goad the immune system to fight the virus, they constructed virus-like particles composed of many copies of one BPV protein. These particles couldn’t cause disease, but they spurred rabbits to crank out antibodies that prevent the viruses from invading cells, the researchers revealed in 1992.
But the scientists hit a wall when they tried to produce virus-like particles with HPV16 proteins. They eventually learned that the hang-up was the specific HPV16 clone that they and most other researchers used, which had been isolated from a patient’s tumor. As Schiller, Lowy, and their colleagues demonstrated in 1993, the protein from other isolated samples of HPV16 could yield ample amounts of virus-like particles.
That discovery paved the way for the development of HPV vaccines, the first of which started reaching patients in 2006. HPV vaccines aren’t the only immunizations that prevent cancer — the hepatitis B vaccine does, as well — but they were the first vaccines exclusively designed to provide that protection, says Schiller. The vaccines have already made an impact. For example, a 2019 study of 14 countries where the vaccines are widely available reported that the frequency of pre-cancerous cervical lesions had fallen by 31% among women between the ages of 20 and 24 and by 51% among girls between 15 and 19 years old. If more people receive the vaccines, they could have an even bigger effect, says Schiller. “They have the potential to essentially eliminate one of the leading causes of cancer in women.”

Nancy Brinker at the 2005 Lasker Awards Luncheon
Nancy Brinker, recipient of a 2005 Lasker Award, left an imprint on cancer research without ever picking up a pipette or sequencing a gene. Brinker started the organization now known as Susan G. Komen in 1982 with a budget of $200. Named for her sister, who died from breast cancer two years before, the foundation has expanded into the largest breast cancer philanthropy, steering $988 million to research and another $2.2 billion to education, treatment, and screening. And Brinker also helped reshape the public’s attitudes toward cancer, which was long regarded as a shameful disease that polite people didn’t discuss. As she wrote in 2005, when her sister fell ill “breast cancer was still a silent epidemic. People called it ‘the Big C’, as if you might catch cancer by just saying the word.”
Through efforts such as the Race for the Cure, public advocacy, and other events, Brinker helped boost awareness of breast cancer and dissolve that stigma.
More than 25 years have passed since Druker opened that box from Nicholas Lydon. Imatinib remains a standby of CML therapy, and patients are receiving dozens of other targeted therapies that it inspired. But the drug almost didn’t happen, Druker says. Other researchers warned him that “a treatment targeting a single genetic abnormality wouldn’t work because cancer is too complicated,” he says. “A lot of people didn’t think this was worth pursuing.”
By Mitchell Leslie

